- c/o Winds of Hope Foundation, Ch. de Montolivet 19, 1006 Lausanne, Suisse
- +41 (0)21 320 77 22
- info@nonoma.org
« Because of its non-transferable nature, noma is not a priority for anyone. Because of its direct link with malnutrition and lack of hygiene, it appears to be an insoluble problem. And yet it is a symbol: the symbol of our imbalanced world, divided between a society of conspicuous consumption and wastage, and populations of starving people, between ultra-sophisticated technologies and total destitution. » Bertrand Piccard
History

In antiquity, Noma was already familiar to doctors such as Hippocrates, Galen, Celsus and Aretaeus of Cappadocia. In Europe, many texts from the 18th and 19th centuries in France, Germany, Poland, Sweden, the Netherlands, Great Britain and Spain mention this disease. Noma cases were also described in the United States in 1826 and 1848. In his dissertation of 1848, “Noma, or sphacellum of the mouth in children”, Jules Tourdes of the Faculty of Medicine in Strasbourg defined noma as a “gangrene that starts in the mouth, and mainly affects children whose general health is weakened by poor hygiene and severe infantile diseases such as eruptive fevers. The attack begins with a mucous ulcer associated with edema of the face and then spreads rapidly from inside to outside, destroying soft tissues and bone. It is almost always fatal”.
In the 20th century, with outbreaks of famine disappearing and good hygiene developing, noma disappeared from the industrialized countries, with the exception of the cases described in the Nazi concentration camps of Auschwitz and Belsen. The campaign led by Edmond Kaiser and Yvan Muriset, founders of Sentinelles, was instrumental in the making people aware that noma had not disappeared everywhere. It was in 1989, at the General Assembly of the World Health Organization (WHO), that noma was put on the international agenda for the first time. In 1992, a major step forward was taken when WHO adopted a strategy and plan of action to combat noma. This was followed in 1994 by the recognition of noma as a public health problem and the establishment of an international program to combat noma, supported by the creation of an “International Network for Action against Noma” (RIACN), which was made responsible for monitoring this program.

In the absence of funding and, unfortunately, also lack of interest on the part of the international community, WHO had to put its program on hold and hand over responsibility to the WHO Regional Office for Africa (WHO/Afro). Only local, privately funded campaigns continued to be carried out, thanks in particular to the NGOs Sentinelles, Hilfsaktion, Campaner, Au Fil de la Vie, Hymne aux Enfants and Enfants du noma. Several surgical missions carried out by volunteer specialists enabled dozens of children to have operations.It was not until 2000 that the intervention of the Winds of Hope Foundation resulted in the revival of the national noma programs initially planned by WHO. Following the successful completion of an experimental pilot project in Niger, the Foundation signed a five-year collaboration agreement with WHO in 2003 to expand its operations in Burkina Faso and Mali, followed by Benin, Togo and Senegal.
Epidemiological monitoring
Reliable data on the number of noma cases is hard to find, given the precarious nature of the health and civil record-keeping systems in the countries where the disease occurs.
The annual distribution of new cases shows that climatic factors play a role. There is a recrudescence during the dry season, renamed the “month of hunger” by some researchers. Another factor that makes it difficult to collect data is that most victims will not have time to arrive in healthcare facilities before succumbing to the disease. So the situation is in fact much worse than it seems.
The annual distribution of new cases shows that climatic factors play a role. There is a recrudescence during the dry season, renamed the “month of hunger” by some researchers. Another factor that makes it difficult to collect data is that most victims will not have time to arrive in healthcare facilities before succumbing to the disease. So the situation is in fact much worse than it seems :
- More than 100,000 children are affected by noma every year. The victims are almost all children aged between 6 months and 6 years. In the absence of treatment, noma is fatal in more than 70 to 90% of cases. A reasonable estimate would be about 80,000 deaths a year.
- 20’000 children a year survive noma, but then live hidden away.
- There are 500,000 noma survivors currently alive in the world.
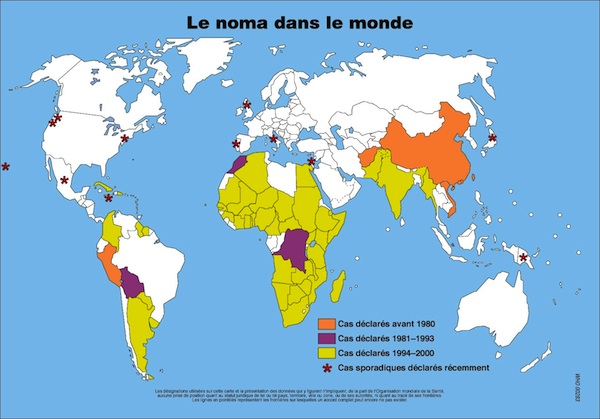
- The poorest countries in Africa, Asia and South America are affected and the African continent is hardest hit, with 80% of the cases.
- Noma, which today is endemic in many African countries, has reached the proportions of a public health problem, especially in certain populations of the Sahel region, a region also designated by some as the «noma belt».
- Noma is reported to be on the rise in Africa, in common with most oral diseases. This is due to a general deterioration in living conditions: malnutrition, poor hygiene, HIV / AIDS, conflict, corruption, etc..
- Noma reappears sporadically in developed countries. Its emergence there is linked to factors such as HIV / AIDS.
This study is based on the only existing available statistics, which were established more than 10 years ago by WHO. Further studies would be desirable.
Studies and research

There is still only very limited literature and research on noma. However, what exists has established that the first symptoms often develop after a child has had an infectious disease, or in a child suffering from malnutrition.
Recent research by GESNOMA (Prof. Denis Montandon and Dr. Denise Baratti-Mayer of the University Hospital of Geneva) has shown that noma is caused by a sharp drop in immune defenses, the origin of which lies in the mother’s state of malnutrition and fatigue during pregnancy, in the presence numerous siblings.
Thesis by Dr Denise Baratti Mayer – Study on etiology of noma
An etiological research project was carried out by the Geneva foundation GESNOMA, to establish whether a specific bacterial or viral agent could be the cause of the disease. The answer was negative – the appearance of noma is not linked to any specific bacterium or virus.
This research was the subject of an article in The Lancet:: Risk factors for noma disease: a 6-years, prospective, matched case-control, study in Niger

